Israel unveils miniature human heart model to transform drug testing
A minuscule model of a human heart, the size of a grain of rice, has been created in Israel. With the potential to put an end to the often criticized animal testing by pharmaceutical companies.
By JUDY SIEGEL-ITZKOVICH, Jerusalem Post, AUGUST 7, 2023
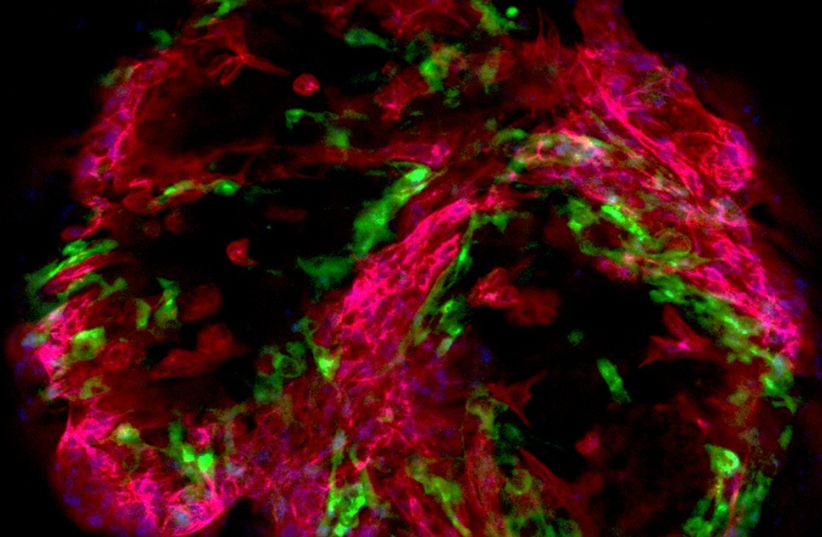
Fluorescent Heart (photo credit: Tissue Dynamics Ltd.)
In a major breakthrough,
a collaborative team of Israeli researchers has unveiled a miniature
human heart model that could potentially transform drug testing and
cardiovascular research, providing alternatives to animal testing. The
self-paced multi-chambered human heart model – no larger than a grain of
rice – promises to revolutionize the way the heart and its functions
are studied.
The team
was led by Yaakov Nahmias, a bioengineering professor from the Hebrew
University of Jerusalem, and included scientists from the
Technion-Israel Institute of Technology in Haifa, and Rehovot-based
Tissue Dynamics Ltd., which is devoted to animal-free drug development.
Their discovery marks “a new era in cardiovascular research,
multi-chambered, self-paced miniature heart model, holding the key to
saving lives and enhancing patient outcomes,” they said in the study.
Sensors also revealed a new mechanism of cardiac arrhythmia not found
in small animals, promising alternatives to animal testing.
This
study, just published in the prestigious Nature Biomedical Engineering,
was entitled “Electro-metabolic coupling in multi-chambered
vascularized human cardiac organoids.”
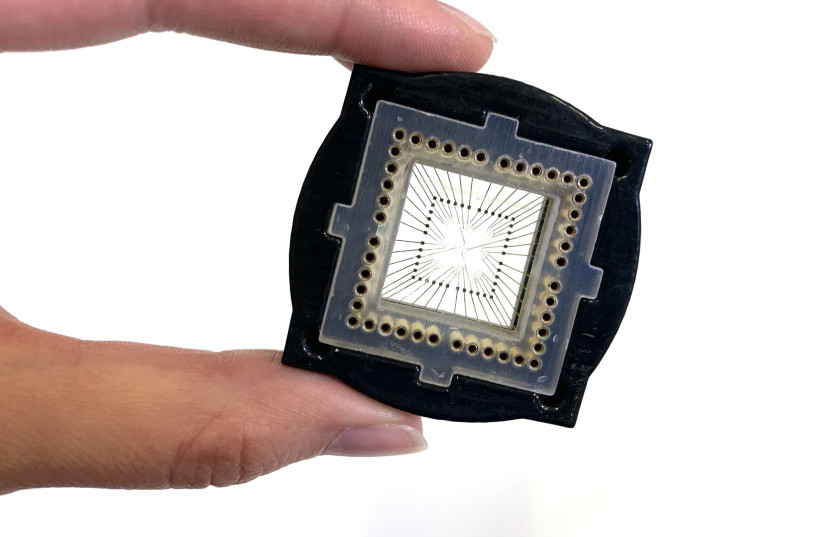
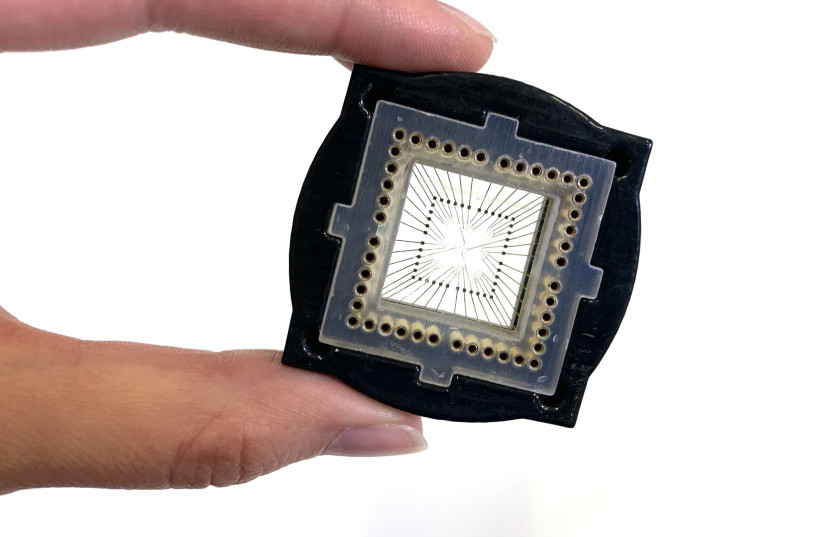 A hand with a microchip (credit: Tissue Dynamics Ltd.)
A hand with a microchip (credit: Tissue Dynamics Ltd.)
Cardiovascular diseases
remain – together with cancers – the leading causes of death around the
world, underscoring the critical importance of their pioneering work.
Nahmias
and his team embarked on an intricate effort to create an accurate
replica of the human heart, using human-induced pluripotent stem cells
(hiPSCs). The resulting model comprises multiple chambers, pacemaker
clusters, epicardial membrane, and endocardial lining, all meticulously
designed to mimic the structure and functions of the human heart.
One of the most significant features of this heart model is its
ability to provide real-time measurements of essential parameters, such
as oxygen consumption, extracellular field potential, and cardiac
contraction. This capability made it possible for the scientists to gain
unprecedented insights into heart function and diseases.
What are the implications for future medical practice?
The
research team has already made groundbreaking discoveries that were
previously unattainable using conventional methods. The tiny heart model
presented a new form of cardiac arrhythmia that is distinct from those
observed in traditional animal models, thus offering new paths for
studying human physiology.
The
implications of this discovery extend to the pharmaceutical industry,
as it allows researchers to gain invaluable insights into the precise
effects of pharmaceutical compounds on the human heart. The heart
model’s response to the chemotherapeutic drug mitoxantrone, which is
commonly used to treat leukemia and multiple sclerosis, was carefully
tested.
Through these
experiments, the researchers pinpointed how mitoxantrone induces
arrhythmia by disrupting the heart’s electro-mitochondrial coupling.
They also discovered a potential solution by administering the common
diabetes drug metformin, which showed promise in mitigating some of the
drug’s adverse effects.
Nahmias,
who is the director of Hebrew University’s Grass Center for
Bioengineering and a fellow of the Royal Society of Medicine and the
American Institute for Medical and Biological Engineering, stressed the
significance of their work.
“The
integration of our complex human heart model with sensors allowed us to
monitor critical physiological parameters in real-time, revealing
intricate mitochondrial dynamics driving cardiac rhythms,” he said. “It
is a new chapter in human physiology.”
The
scientists partnered with Tissue Dynamics, which focuses on reducing
research and development costs for drugs by 30% to 80% by providing
groundbreaking drug toxicity and efficacy tools for the pharmaceutical industry.
Its proprietary screening platform uses tissue-embedded microsensors in
a micro-physiological environment to monitor changes in tissue function
in real-time.
The
Nachmias team developed a robotic system that can screen 20,000 tiny
human hearts in parallel for applications to drug discoveries. The
potential applications of this micro-physiological system are huge,
promising to enhance our understanding of heart physiology and speed up
the discovery of safer and more effective pharmaceutical interventions
and leading to a healthier future for all.
“This
miniature-yet-sophisticated human heart model has the potential to
reshape drug testing practices, advance our understanding of
cardiovascular diseases, and ultimately contribute to a healthier and
more sustainable future.”
The Researchers
By offering unparalleled accuracy and insights into cardiovascular
diseases, this advanced human heart model has the potential to
revolutionize drug-testing methodologies. With this tiny heart model,
researchers are poised to make significant strides in developing safer
and more effective medications for patients worldwide, potentially
saving lives and improving patient outcomes.
The
miniature heart model also presents an ethical advantage, as it offers a
viable alternative to animal testing. This breakthrough could mark a
turning point in the pharmaceutical industry, reducing reliance on
animal models and minimizing potential harm to animals in the pursuit of
medical advancements.
The
scientists concluded that their tiny heart represents a monumental
achievement with far-reaching implications for medical research.
“This
miniature-yet-sophisticated human heart model has the potential to
reshape drug testing practices, advance our understanding of
cardiovascular diseases, and ultimately contribute to a healthier and
more sustainable future,” they wrote".
PLEASE RECOMMEND THIS PAGE AND FOLLOW US AT
In a major breakthrough, a collaborative team of Israeli researchers has unveiled a miniature human heart model that could potentially transform drug testing and cardiovascular research, providing alternatives to animal testing. The self-paced multi-chambered human heart model – no larger than a grain of rice – promises to revolutionize the way the heart and its functions are studied.
The team was led by Yaakov Nahmias, a bioengineering professor from the Hebrew University of Jerusalem, and included scientists from the Technion-Israel Institute of Technology in Haifa, and Rehovot-based Tissue Dynamics Ltd., which is devoted to animal-free drug development.
Their discovery marks “a new era in cardiovascular research, multi-chambered, self-paced miniature heart model, holding the key to saving lives and enhancing patient outcomes,” they said in the study.
Sensors also revealed a new mechanism of cardiac arrhythmia not found in small animals, promising alternatives to animal testing.
This study, just published in the prestigious Nature Biomedical Engineering, was entitled “Electro-metabolic coupling in multi-chambered vascularized human cardiac organoids.”
Cardiovascular diseases remain – together with cancers – the leading causes of death around the world, underscoring the critical importance of their pioneering work.
Nahmias and his team embarked on an intricate effort to create an accurate replica of the human heart, using human-induced pluripotent stem cells (hiPSCs). The resulting model comprises multiple chambers, pacemaker clusters, epicardial membrane, and endocardial lining, all meticulously designed to mimic the structure and functions of the human heart.
One of the most significant features of this heart model is its ability to provide real-time measurements of essential parameters, such as oxygen consumption, extracellular field potential, and cardiac contraction. This capability made it possible for the scientists to gain unprecedented insights into heart function and diseases.
What are the implications for future medical practice?
The research team has already made groundbreaking discoveries that were previously unattainable using conventional methods. The tiny heart model presented a new form of cardiac arrhythmia that is distinct from those observed in traditional animal models, thus offering new paths for studying human physiology.
The implications of this discovery extend to the pharmaceutical industry, as it allows researchers to gain invaluable insights into the precise effects of pharmaceutical compounds on the human heart. The heart model’s response to the chemotherapeutic drug mitoxantrone, which is commonly used to treat leukemia and multiple sclerosis, was carefully tested.
Through these experiments, the researchers pinpointed how mitoxantrone induces arrhythmia by disrupting the heart’s electro-mitochondrial coupling. They also discovered a potential solution by administering the common diabetes drug metformin, which showed promise in mitigating some of the drug’s adverse effects.
Nahmias, who is the director of Hebrew University’s Grass Center for Bioengineering and a fellow of the Royal Society of Medicine and the American Institute for Medical and Biological Engineering, stressed the significance of their work.
“The integration of our complex human heart model with sensors allowed us to monitor critical physiological parameters in real-time, revealing intricate mitochondrial dynamics driving cardiac rhythms,” he said. “It is a new chapter in human physiology.”
The scientists partnered with Tissue Dynamics, which focuses on reducing research and development costs for drugs by 30% to 80% by providing groundbreaking drug toxicity and efficacy tools for the pharmaceutical industry. Its proprietary screening platform uses tissue-embedded microsensors in a micro-physiological environment to monitor changes in tissue function in real-time.
The Nachmias team developed a robotic system that can screen 20,000 tiny human hearts in parallel for applications to drug discoveries. The potential applications of this micro-physiological system are huge, promising to enhance our understanding of heart physiology and speed up the discovery of safer and more effective pharmaceutical interventions and leading to a healthier future for all.
“This miniature-yet-sophisticated human heart model has the potential to reshape drug testing practices, advance our understanding of cardiovascular diseases, and ultimately contribute to a healthier and more sustainable future.”
The Researchers
By offering unparalleled accuracy and insights into cardiovascular diseases, this advanced human heart model has the potential to revolutionize drug-testing methodologies. With this tiny heart model, researchers are poised to make significant strides in developing safer and more effective medications for patients worldwide, potentially saving lives and improving patient outcomes.
The miniature heart model also presents an ethical advantage, as it offers a viable alternative to animal testing. This breakthrough could mark a turning point in the pharmaceutical industry, reducing reliance on animal models and minimizing potential harm to animals in the pursuit of medical advancements.
The scientists concluded that their tiny heart represents a monumental achievement with far-reaching implications for medical research.
“This miniature-yet-sophisticated human heart model has the potential to reshape drug testing practices, advance our understanding of cardiovascular diseases, and ultimately contribute to a healthier and more sustainable future,” they wrote".

No comments:
Post a Comment
Stick to the subject, NO religion, or Party politics